Maternal mortality is a significant public health issue in the United States, where pregnancy-related deaths are alarmingly on the rise. Over the past few years, the nation has led its high-income counterparts in maternal mortality rates, with studies revealing that more than 80% of these fatalities are preventable. The impact of COVID-19 on pregnancy has only exacerbated healthcare disparities, contributing to the steep increase in pregnancy-related deaths. Racial and ethnic inequities have further complicated the picture, highlighting the urgent need for improved postpartum care and comprehensive maternal health strategies. This crisis necessitates a collective response to enhance healthcare access and ultimately reduce preventable maternal mortality rates, ensuring that every mother has the chance for a healthy pregnancy and safe delivery.
The term “maternal mortality” encompasses a critical aspect of women’s health, particularly concerning the deaths that occur during pregnancy or shortly after childbirth. Often referred to as pregnancy-related fatalities, these occurrences underline the vulnerabilities faced by women throughout their maternal journey. The disparities observed in maternal health outcomes, especially among different racial and ethnic groups, raise significant concerns about access to quality medical care and postpartum support. Furthermore, understanding the effects of crises like the COVID-19 pandemic on maternal health is vital in creating targeted interventions. Addressing these issues through equitable healthcare solutions is essential to protect maternal well-being and reduce the incidence of such tragedies.
Understanding Maternal Mortality Rates in the U.S.
Maternal mortality rates in the United States present a concerning trend, as they have been increasing over recent years, particularly between 2018 and 2022. Despite being a high-income country, the U.S. leads its peers with the highest rates of pregnancy-related deaths, primarily attributed to preventable causes. Factors contributing to this alarming statistic include systemic issues within healthcare, such as inadequate access to prenatal care and socio-economic disparities that affect different racial and ethnic groups disproportionately. American Indian, Alaska Native, and Black women, for example, represent groups with persistently high maternal mortality rates, indicating significant healthcare inequities that must be addressed to lower these figures.
The continued rise in maternal mortality rates highlights a pressing need for comprehensive reforms in maternal health policies. A critical analysis of the healthcare system reveals the importance of increasing access to quality care, particularly throughout the extended postpartum period. By focusing on interventions aimed at reducing healthcare disparities, we can shift the trajectory of maternal mortality, aiming for a future where all women receive the necessary support during and after pregnancy. Initiatives that prioritize maternal health equity could lead to substantial improvements in outcomes for the most vulnerable populations.
The Role of Postpartum Care in Reducing Maternal Deaths
Postpartum care is a crucial, yet often overlooked, aspect of maternal health, contributing significantly to the rates of maternal mortality in the U.S. A staggering one-third of maternal deaths occur after the immediate postpartum period, underscoring the necessity for healthcare systems to provide ongoing support and monitoring beyond the typical six-week check-up. Implementing comprehensive postpartum care programs can ensure that women are not only physically healed after childbirth but also receive mental health support, education on warning signs for complications, and access to resources that promote overall wellness in the postpartum phase.
To address the gap in postpartum care, it’s essential to shift the focus from a short-term view of recovery to a continuous care model that spans the first year after childbirth. This approach recognizes that the postpartum period should not be confined to a ‘cliff’ ending. By fostering a healthcare environment where extended support is readily available, we can drastically improve outcomes for maternal health and significantly reduce the number of preventable maternal deaths. Addressing postpartum care as a priority within maternal health will ultimately lead to healthier outcomes for mothers and their families.
The Disparities in Maternal Health Across Racial and Ethnic Groups
The study of maternal mortality rates in the U.S. reveals stark disparities among racial and ethnic groups that cannot be ignored. Research indicates that American Indian and Alaska Native women experience maternal mortality rates that are nearly four times higher than those of white women. Non-Hispanic Black women also face significantly higher risks, showcasing a troubling intersection of healthcare disparities and systemic inequities that persist across the country. Such disparities highlight urgent calls to action for policymakers and healthcare providers to ensure that all women receive equitable maternal care, regardless of their race or background.
Addressing these disparities requires a multifaceted approach, including a thorough evaluation of the social determinants of health that contribute to unequal treatment outcomes. Moreover, targeted interventions must be developed to eliminate bias within healthcare settings and to provide culturally competent care. Only through sustained efforts to dismantle barriers can we hope to achieve improvements in maternal health across all demographics, ultimately leading to a reduction in the alarming rates of maternal mortality.
Impact of COVID-19 on Pregnancy and Maternal Health
The COVID-19 pandemic has significantly impacted maternal health, contributing to a rise in pregnancy-related deaths from 2018 to 2022. Research indicated that the sharpest increase in maternal mortality coincided with the initial outbreak of the pandemic. The interplay between stressors such as job loss, healthcare access challenges, and increased chronic health issues among reproductive-age individuals has collectively worsened pregnancy outcomes. The pandemic revealed the vulnerabilities within the maternity care system, amplifying existing problems in access to quality care and raising new challenges that need to be addressed urgently.
As we navigate the aftermath of the pandemic, it is critical for healthcare systems to assess and adapt to the lessons learned during this time. This includes enhancing communication with expectant and postpartum mothers about the risks associated with COVID-19 and its implications for pregnancy. Additionally, addressing the mental health crisis exacerbated by the pandemic is vital to ensure that mothers receive comprehensive support. By focusing on the key lessons learned from COVID-19, we can implement improved strategies to bolster maternal health outcomes and create resilient systems that are prepared for future public health challenges.
The Importance of Comprehensive Prenatal Care
Comprehensive prenatal care is vital for reducing maternal mortality rates and ensuring healthy pregnancy outcomes. The majority of pregnancy-related deaths are preventable, yet many women lack access to the prenatal services and support necessary for a healthy pregnancy journey. Early and regular prenatal visits allow for the detection and management of potential complications, including chronic conditions such as hypertension or diabetes. By improving access to these essential services, we can significantly reduce risks associated with pregnancy-related deaths and promote better maternal health.
Incorporating educational components into prenatal care can empower women with knowledge about their bodies and potential complications. This can include guidance on recognizing warning signs during and after pregnancy, emphasizing the importance of follow-up care and the need for open communication with healthcare providers. The commitment to expanding comprehensive prenatal care reflects a broader investment in maternal health, which ultimately promises to save lives and enhance the healthcare experience for mothers.
Policy Changes Needed to Improve Maternal Health Outcomes
To tackle the soaring rates of maternal mortality in the U.S., significant policy changes are essential. Policymakers must address healthcare disparities by ensuring that maternal health initiatives are inclusive and equitable for women from all backgrounds. This includes increasing funding for maternal health programs that cater to underrepresented communities and emphasizing the importance of quality care throughout pregnancy and the postpartum period. With the right policies in place, states can begin to emulate the more successful outcomes seen in regions like California, where maternal health initiatives are more robust.
Furthermore, advocacy for systemic change can help dismantle barriers that prevent access to quality maternal healthcare. Engaging in conversations about public health funding and the prioritization of maternal health during legislative sessions can lead to consequential reforms. These efforts must be sustained, reflecting a commitment to improve the health of all reproductive-age individuals and prioritize their wellbeing through legislation that encourages comprehensive maternal care.
Innovative Solutions to Address Maternal Health Challenges
Innovation plays a crucial role in addressing the complex challenges of maternal health. By leveraging technology, healthcare systems can provide better monitoring and support for mothers at risk of complications during and after pregnancy. For example, telehealth services can improve access to care for women living in maternity care deserts, ensuring that they receive timely and adequate prenatal and postpartum support. Such innovations can bridge gaps in healthcare access, making it more feasible for women to adhere to recommended care protocols.
Moreover, community-based interventions that engage and empower women can lead to improved health outcomes. Programs designed to provide education about maternal health and connect women with local resources can foster a supportive environment that encourages proactive health management. By promoting such programs alongside technological advancements, we create an ecosystem that prioritizes maternal health and responds effectively to the increasing rates of pregnancy-related deaths.
Collaboration Across Sectors to Enhance Maternal Health
Collaboration across various sectors is essential for tackling the multifaceted nature of maternal health challenges. Healthcare providers, policymakers, community organizations, and advocacy groups must unite to create comprehensive strategies that address disparities in maternal mortality. This collaborative approach can lead to the development of integrative policies that enhance access to care, improve quality standards, and prioritize maternal health equity. Engaging multiple stakeholders ensures a wider range of perspectives and resources are brought to the table, fostering a more holistic response to the crisis.
In addition, fostering partnerships with organizations that specialize in addressing social determinants of health can bolster efforts to improve maternal health outcomes. Initiatives that address housing, nutrition, and transportation can create a supportive framework for expecting mothers, thereby improving overall health and potentially reducing complications during pregnancy. As stakeholders work together, the impact of their combined efforts can lead to substantial progress in reducing maternal mortality rates and redefining what maternal health means in the U.S.
Frequently Asked Questions
What are the primary factors contributing to high maternal mortality rates in the U.S.?
The U.S. faces high maternal mortality rates due to multiple factors including disparities in healthcare access, a patchwork healthcare system, and persistent bias and discrimination against racial and ethnic groups. Additionally, an increase in chronic health conditions like cardiovascular diseases among pregnant individuals contributes significantly to pregnancy-related deaths.
How do healthcare disparities affect maternal mortality rates?
Healthcare disparities contribute to heightened rates of maternal mortality by creating unequal access to prenatal and postpartum care. Inadequate healthcare resources and services, especially in rural or marginalized communities, exacerbate these disparities, leading to higher risks of complications during and after pregnancy.
What role does postpartum care play in maternal mortality?
Postpartum care is crucial for maternal health as evidence shows that nearly one-third of pregnancy-related deaths in the U.S. occur in the year following childbirth. Effective postpartum care should ideally extend beyond the first six weeks, addressing ongoing health issues and ensuring adequate support for new mothers.
How has the COVID-19 pandemic impacted maternal mortality rates?
The onset of the COVID-19 pandemic has been associated with a rise in maternal mortality rates, particularly in 2021. Disruptions in healthcare access, increased stress, and the strain on the healthcare system may have contributed to poorer outcomes for pregnant individuals during this time.
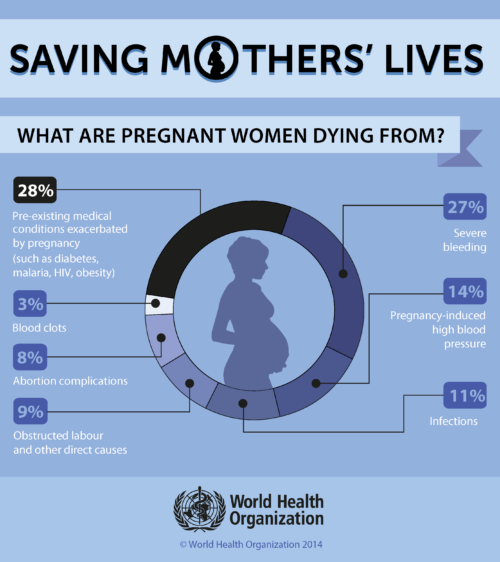
What are the leading causes of pregnancy-related deaths in the U.S.?
Cardiovascular disease has emerged as the leading cause of pregnancy-related deaths, accounting for over 20% of these fatalities. Other significant causes include hemorrhage and hypertensive disorders, showcasing the need for targeted healthcare interventions to manage chronic conditions effectively.
Can maternal mortality rates be reduced within a year after childbirth?
Yes, reducing maternal mortality rates within the year after childbirth is feasible through improved postpartum care and health systems designed to monitor and address women’s health well beyond the initial weeks after birth. Enhanced access to ongoing care and support systems can significantly lower risks.
Why is monitoring late maternal deaths important for maternal health outcomes?
Monitoring late maternal deaths is essential as it highlights the continuum of care needed post-pregnancy. By recognizing and addressing health risks for up to a year after childbirth, healthcare systems can improve maternal health outcomes and better support women during their recovery.
What strategies are being discussed to improve maternal health in the U.S.?
Strategies to improve maternal health include increasing investments in public health infrastructure, enhancing quality of prenatal and postpartum care, and addressing policy differences that lead to state-level disparities in maternal mortality rates. Innovative solutions in healthcare can help reduce preventable deaths among mothers.
| Key Points | Details |
|---|---|
| Rising Maternal Mortality | The U.S. has the highest maternal mortality rate among high-income countries, with it continuing to rise from 2018 to 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths in the U.S. are preventable, highlighting deficiencies in prenatal and postpartum care. |
| Disparities by Race | Significant racial disparities exist, with American Indian and Alaska Native women facing the highest mortality rates. |
| Covid-19 Impact | The COVID-19 pandemic exacerbated maternal mortality rates, particularly in 2021. |
| Leading Causes of Death | Cardiovascular disease is the leading cause of pregnancy-related deaths, surpassing hemorrhage. |
| Late Maternal Deaths | Nearly a third of maternal deaths occur between 42 days and 1 year postpartum, warranting broader definitions of maternal mortality. |
| Public Health Infrastructure | Investment in public health infrastructure and innovative care solutions is critical to improve maternal health outcomes. |
Summary
Maternal mortality remains a pressing issue, particularly in the United States where rates are alarmingly high compared to other high-income nations. Recent studies reveal that more than 80 percent of pregnancy-related deaths are preventable, emphasizing the urgent need for improved prenatal and postpartum care. Addressing disparities based on race and state is crucial, as many of these deaths are avoidable with better healthcare policies and infrastructure. As we move forward, focusing on chronic health conditions and extending care beyond the initial weeks postpartum will be vital to combat the rise in maternal mortality.